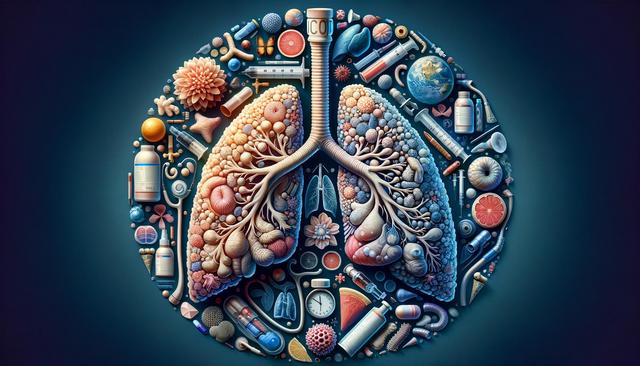
What is COPD and How Does It Affect the Lungs?
COPD, or Chronic Obstructive Pulmonary Disease, is an umbrella term for a group of progressive lung diseases, the most common of which are emphysema and chronic bronchitis. These conditions cause airflow blockage and breathing-related issues, often due to long-term exposure to irritating gases or particulate matter, most commonly from cigarette smoke. Over time, the airways and air sacs in the lungs lose their elasticity and become inflamed, leading to symptoms such as chronic cough, mucus production, and shortness of breath. These symptoms tend to worsen gradually, impacting everyday activities and quality of life.
In people with COPD, the damage to the lungs is largely irreversible, but early diagnosis and proper management can help slow the progression. The condition affects millions worldwide and is a leading cause of disability. Understanding its mechanisms is essential for recognizing symptoms early and seeking timely medical advice.
Common Symptoms and Risk Factors
Identifying the signs of COPD early on is key to managing the condition effectively. The symptoms can vary depending on the severity of the disease but often include:
- Persistent coughing, often with mucus (chronic bronchitis)
- Shortness of breath, especially during physical activities
- Wheezing and chest tightness
- Frequent respiratory infections
- Fatigue and reduced exercise tolerance
The primary risk factor for COPD is long-term smoking. However, other contributors include exposure to air pollutants, occupational dust and chemicals, and a genetic condition known as alpha-1 antitrypsin deficiency. Age also plays a role, as symptoms typically appear in people aged 40 and older. While smoking remains the most significant preventable risk, non-smokers can also develop COPD due to environmental and genetic factors.
Diagnosis and Medical Evaluation
Early diagnosis of COPD can significantly improve outcomes and slow disease progression. Physicians typically begin with a review of symptoms and medical history, followed by a physical examination. To confirm a diagnosis, a key test used is spirometry, which measures lung function by evaluating how much air a person can inhale and exhale, and how quickly.
Other diagnostic tools may include:
- Chest X-rays or CT scans
- Arterial blood gas analysis to measure oxygen levels
- Lab tests to rule out other conditions or identify genetic causes
Accurate diagnosis helps differentiate COPD from other respiratory issues like asthma or heart failure. It also enables healthcare providers to tailor a treatment plan that addresses the individual’s specific needs, lifestyle, and disease stage.
Treatment Options and Lifestyle Adjustments
While there is no cure for COPD, several treatment strategies can help manage symptoms and improve quality of life. These typically include a combination of medications, pulmonary rehabilitation, and lifestyle changes. Common treatments involve:
- Bronchodilators to relax the muscles around the airways
- Inhaled steroids to reduce inflammation
- Combination inhalers for more comprehensive symptom control
- Oxygen therapy for those with low blood oxygen levels
In more severe cases, surgical interventions such as lung volume reduction surgery or, rarely, lung transplantation may be considered. However, beyond medical treatments, lifestyle changes play a crucial role. Quitting smoking is the most effective step in slowing COPD progression. Additionally, staying active, eating a balanced diet, and managing stress can help patients maintain better overall health and lung function.
Living with COPD: Coping Strategies and Support
Managing life with COPD involves more than just taking medication—it requires a holistic approach that includes emotional and social support. Living with a chronic illness can be challenging, but many find that building a support system and staying informed can make a significant difference. Pulmonary rehabilitation programs offer structured education, exercise training, and nutritional advice tailored to people with lung conditions.
Some effective coping strategies include:
- Joining a COPD support group to share experiences and gain encouragement
- Learning breathing techniques like pursed-lip breathing
- Monitoring symptoms and keeping regular medical appointments
- Using air purifiers to reduce indoor air pollution
Family involvement and caregiver support are also essential, as they can assist with daily tasks and provide emotional encouragement. With the right resources and a proactive approach, individuals with COPD can continue to lead fulfilling lives.
Conclusion: Taking Control of COPD
Understanding COPD is the first step toward managing it effectively. While it is a progressive condition, early diagnosis, appropriate treatment, and lifestyle changes can significantly improve daily functioning and overall well-being. For those living with COPD, staying informed, maintaining open communication with healthcare providers, and accessing support networks are essential components of long-term management. By taking active steps toward better lung health, individuals can navigate the challenges of COPD with greater confidence and resilience.



Leave a Reply