What is Amyloidosis and How Does It Develop?
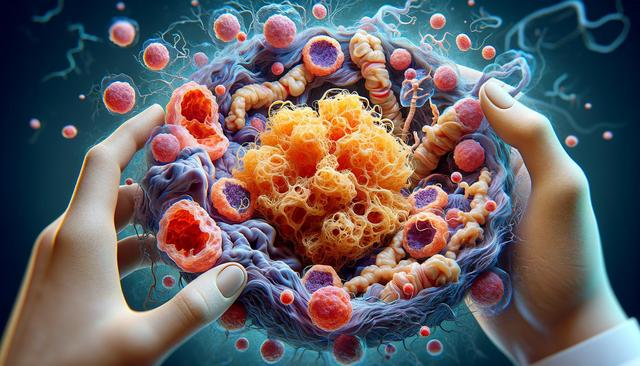
To fully understand amyloidosis, it’s important to answer the question: what is amyloidosis? This condition involves the accumulation of abnormal protein deposits, known as amyloid, in different organs and tissues throughout the body. These proteins are typically produced in the bone marrow and can be deposited in any area, including the heart, kidneys, liver, spleen, nervous system, and digestive tract. Over time, the buildup of amyloid can interfere with the normal function of these organs, leading to serious health complications.
Amyloidosis can be classified into several types, depending on the protein involved. The main types include:
- AL (primary) amyloidosis, which occurs when abnormal light chain proteins are produced by bone marrow cells.
- AA (secondary) amyloidosis, usually triggered by chronic infections or inflammatory diseases.
- Hereditary amyloidosis, caused by inherited gene mutations.
- Dialysis-related amyloidosis, associated with long-term dialysis treatment.
Each type of amyloidosis has distinct causes and may require different treatment approaches. Early diagnosis is crucial to managing the disease and preventing organ damage.
Recognizing Amyloidosis Warning Signs
Identifying amyloidosis warning signs early can make a significant difference in treatment outcomes. Unfortunately, because symptoms vary widely and resemble other conditions, amyloidosis is often misdiagnosed or discovered late. Individuals should monitor for persistent or unexplained health changes, especially if they have risk factors such as chronic inflammatory diseases or a family history of amyloidosis.
Common warning signs include:
- Unexplained weight loss
- Severe fatigue or weakness
- Shortness of breath
- Swelling in the legs or ankles
- Numbness or tingling in hands and feet
- Irregular heartbeat
These symptoms, while nonspecific, should prompt medical evaluation if they persist without clear cause. When multiple symptoms appear together, especially in individuals with known risk factors, further investigation for amyloidosis may be necessary.
Understanding Amyloidosis Symptoms by Affected Area
Amyloidosis symptoms can vary significantly based on the organs affected. This variability is one of the reasons why the disease can be difficult to diagnose. For instance, amyloid deposits in the kidneys may lead to nephrotic syndrome, while deposits in the heart can result in restrictive cardiomyopathy.
Some examples of organ-specific symptoms include:
- Kidneys: Foamy urine, swelling (edema), reduced kidney function
- Heart: Irregular heartbeat, chest pain, difficulty breathing
- Liver and spleen: Abdominal discomfort, enlarged organs
- Nervous system: Numbness, pain in hands and feet, dizziness upon standing
It’s also important to note that amyloidosis symptoms may overlap with those of other chronic illnesses, which can delay diagnosis. Healthcare providers often need to perform a series of imaging tests, blood work, and tissue biopsies to confirm amyloidosis and determine the specific type.
Amyloidosis and Skin Manifestations
While internal organ involvement is more common, amyloidosis can sometimes manifest through changes in the skin. These skin symptoms can serve as external clues to an internal condition. When investigating visible signs, healthcare professionals may refer to amyloidosis skin pictures to differentiate these symptoms from other dermatological conditions.
Skin-related symptoms of amyloidosis may include:
- Purplish patches around the eyes (so-called ‘raccoon eyes’)
- Waxy, thickened skin texture
- Easy bruising, particularly in the upper chest and neck areas
- Small, raised bumps or nodules
Though these symptoms are less common, they are often associated with AL amyloidosis. If you notice unexplained skin changes, especially in combination with other systemic issues, it’s important to consult with a healthcare provider for further evaluation.
Diagnosis and Management of Amyloidosis
Diagnosing amyloidosis involves a combination of medical history, physical examination, imaging techniques, and laboratory tests. A definitive diagnosis often requires a biopsy of affected tissue, where amyloid deposits can be identified through special staining techniques. Genetic testing may also be used for hereditary forms of the disease.
Management of amyloidosis depends on the type and severity of the condition. Treatment goals typically focus on reducing the production of amyloid-forming proteins and managing organ damage. Therapeutic options may include:
- Medications to control the underlying cause (e.g., chemotherapy for AL amyloidosis)
- Supportive care to manage symptoms (e.g., diuretics for fluid retention)
- Organ-specific interventions, such as dialysis for kidney failure
- Stem cell transplant in select cases
Because amyloidosis is a complex condition, ongoing monitoring and a multidisciplinary care approach are essential. Early intervention can slow disease progression and improve quality of life.



Leave a Reply